Sleep is crucial to health, but for many women, peaceful nighttime sleep is frequently interrupted without apparent reason. One silent but serious culprit is sleep apnea in women, a disorder that often remains undiagnosed. While long viewed as a male-predominant disorder, mounting evidence indicates that women are also profoundly affected—albeit in differing ways.
According to the American Academy of Sleep Medicine, nearly 17% of women have obstructive sleep apnea (OSA), with the true prevalence much higher due to underdiagnosis. As women tend to have less severe symptoms than men, awareness and prompt evaluation are essential.
Dr. Manu Madan, a well-known pulmonologist from Saket, Delhi, has been pioneering sleep medicine. With over a decade of clinical experience behind him, he observes, “Many women aren’t aware that chronic fatigue, insomnia, or mood swings can be symptoms of sleep apnea. Awareness of the atypical presentation in women can alter the course of care.”
What is Sleep Apnea?
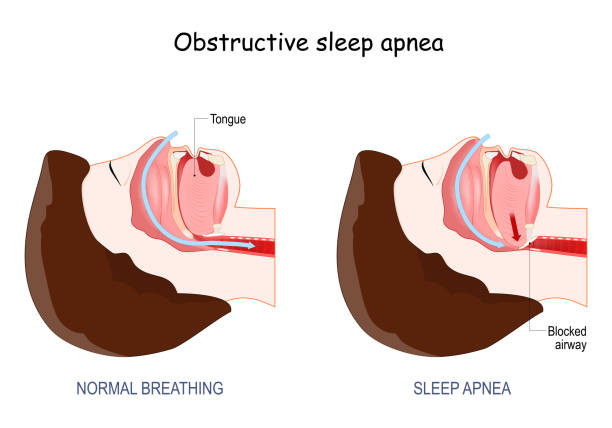
Sleep apnea is a sleep disorder that is defined by repeated periods of interrupted breathing while asleep. The interruptions, or apneas, can range from a few seconds to one minute and can happen several times an hour. Obstructive sleep apnea (OSA) is the most prevalent type, in which the airway collapses or gets blocked. Central sleep apnea (CSA) and complex sleep apnea syndrome (the combination of OSA and CSA) are rarer forms.
These respiratory interruptions cause disjointed sleep and lower blood oxygen levels, which can cause a chain of medical issues over time.
Let’s find out.
Why Sleep Apnea is Different in Women?
Conventionally, sleep apnea among women has gone unrecognized. As opposed to men who present with loud snoring and observed apneas, women present with symptoms that can be confused with other conditions, including depression, anxiety, or insomnia.
Hormonal levels also come into play. During pregnancy, menopause, and even menstrual cycle, hormonal shifts can influence airway stability. Estrogen and progesterone are found to influence upper airway muscles, i.e., increased or decreased levels can exacerbate or initiate sleep apnea.
Women are also more likely to have REM-related sleep apnea, meaning interruptions take place during specific stage of sleep—making them more difficult to identify at shorter diagnostic tests.
Do not ignore subtle health signals.
Common Signs & Symptoms of Sleep Apnea in Women
As opposed to the stereotypical gasping and snoring in men, sleep apnea symptoms in women tend to be more subtle:
- Persistent fatigue and excessive daytime sleepiness
- Recurrent nighttime awakenings
- Insomnia or difficulty falling/staying asleep
- Headaches in the morning
- Irritability or mood swings
- Memory impairments and poor concentration
- Dry mouth or sore throat upon waking up
- Night sweats

Take note that women are also more likely to report symptoms of depression, anxiety, and restless legs, which would make diagnostic resolution more complicated.
Don’t delay until symptoms worsen.
Risks of Untreated Sleep Apnea in Women
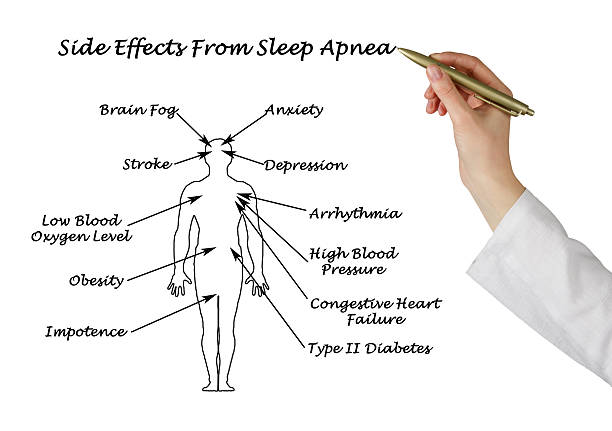
Untreated sleep apnea may lead to serious health consequences, including:
- Cardiovascular disorders: Elevated risk of hypertension, stroke, and heart disease
- Metabolic disorders: Close correlation with insulin resistance and type 2 diabetes
- Hormonal imbalances: Particularly during pregnancy and menopause
- Mental health disorders: Exacerbation of anxiety, depression, and cognitive decline
- Reduced quality of life: Fatigue can compromise work, relationships, and happiness
Current research indicates that women with unmanaged sleep apnea could be at greater risk of developing Alzheimer’s disease because chronic oxygen deficiency impairs brain function.
How Sleep Apnea is Diagnosed

Diagnosis often starts with a thorough sleep history and physical exam. Equipment includes:
- Polysomnography (PSG): A nighttime sleep study done in a sleep lab to track breathing patterns, oxygen, heart rate, and more.
- Home sleep apnea test (HSAT): A handy, portable test taken in the comfort of home, usually used when moderate to severe OSA is suspected.
- Questionnaires: Instruments such as the Epworth Sleepiness Scale or STOP-BANG aid in the recognition of vulnerable individuals.
Dr. Manu Madan stresses, “Diagnosis is important. Even mild sleep apnea can have major health consequences if left untreated.”
Explore the treatment options that can make you breathe easy.
Treatment Options for Women

Sleep apnea in women treatment options are customized and may include:
- Continuous positive airway pressure (CPAP) therapy: The most effective, providing constant airflow to maintain airway patency while asleep.
- Oral appliances: Custom-fitted devices that reposition the jaw or tongue to keep the airway open—particularly helpful for mild to moderate OSA.
- Lifestyle modification: Weight reduction, no alcohol or sedative use, and positional therapy may decrease severity.
- Surgery: In select individuals, UPPP (uvulopalatopharyngoplasty) or Inspire therapy might be an option.
- Hormonal assessment: Addressing hormonal deficiency in menopausal women can provide adjunct benefit.
Try these to enhance your sleep quality.
Tips for Better Sleep if You Suspect Sleep Apnea

If you have sleep apnea symptoms in women, try the following tips:
- Sleep on your side: Less airway obstruction than sleeping on your back.
- Prop your head up: Use a wedge pillow or an adjustable bed to help you breathe.
- Maintain a healthy weight: Overweight is a big risk factor; even modest weight loss will help.
- Make your bedroom sleep-friendly: Keep it cool, dark, and quiet.
- Don’t drink alcohol or have a heavy meal at night: These tend to relax muscles in the throat and make apneas worse.
- Manage stress: Yoga, meditation, or light exercise can reduce sleep-disrupting stress.
These modifications won’t substitute medical treatment but can maximize its effectiveness and promote long-term well-being.
Frequently Asked Questions
Can sleep apnea occur in young women or only after menopause?
Sleep apnea can affect women of all ages. Hormonal changes during menopause increase the risk, but young women, especially those with obesity or PCOS, are also vulnerable.
Is it necessary to use a CPAP machine forever?
Not always. With successful weight loss, lifestyle modification, or other therapies such as oral appliances, some women may decrease or stop CPAP under medical supervision.
Can pregnancy make sleep apnea worse in women?
Yes. Weight gain due to pregnancy and hormonal changes may elevate the risk for developing or aggravating OSA. Proper monitoring is necessary to prevent adverse effects on maternal and fetal well-being.
How long does it take to see improvement after initiating treatment?
Many women report improved sleep quality and decreased fatigue within a few days of CPAP initiation or oral appliance use. Full benefits take several weeks.
Is treatment gender-specific?
Yes. As women may present differently, treatment plans are frequently individualized to treat hormonal, anatomical, and psychological differences.

